CHICAGO —
Summer travel is helping fuel a COVID surge across California and other parts of the country.
There are growing reports of attendees at the Democratic National Convention getting COVID-19. At least a dozen people from California — delegates, political strategists and news reporters — said they tested positive after the DNC ended last week in Chicago.
Democratic strategist Tracy Austin, who caught COVID while attending the convention, told The Times: “It was an amazing time, but the DNCC last week stood for the Democratic National COVID Convention.”
The next big test for the COVID spike is just around the corner.
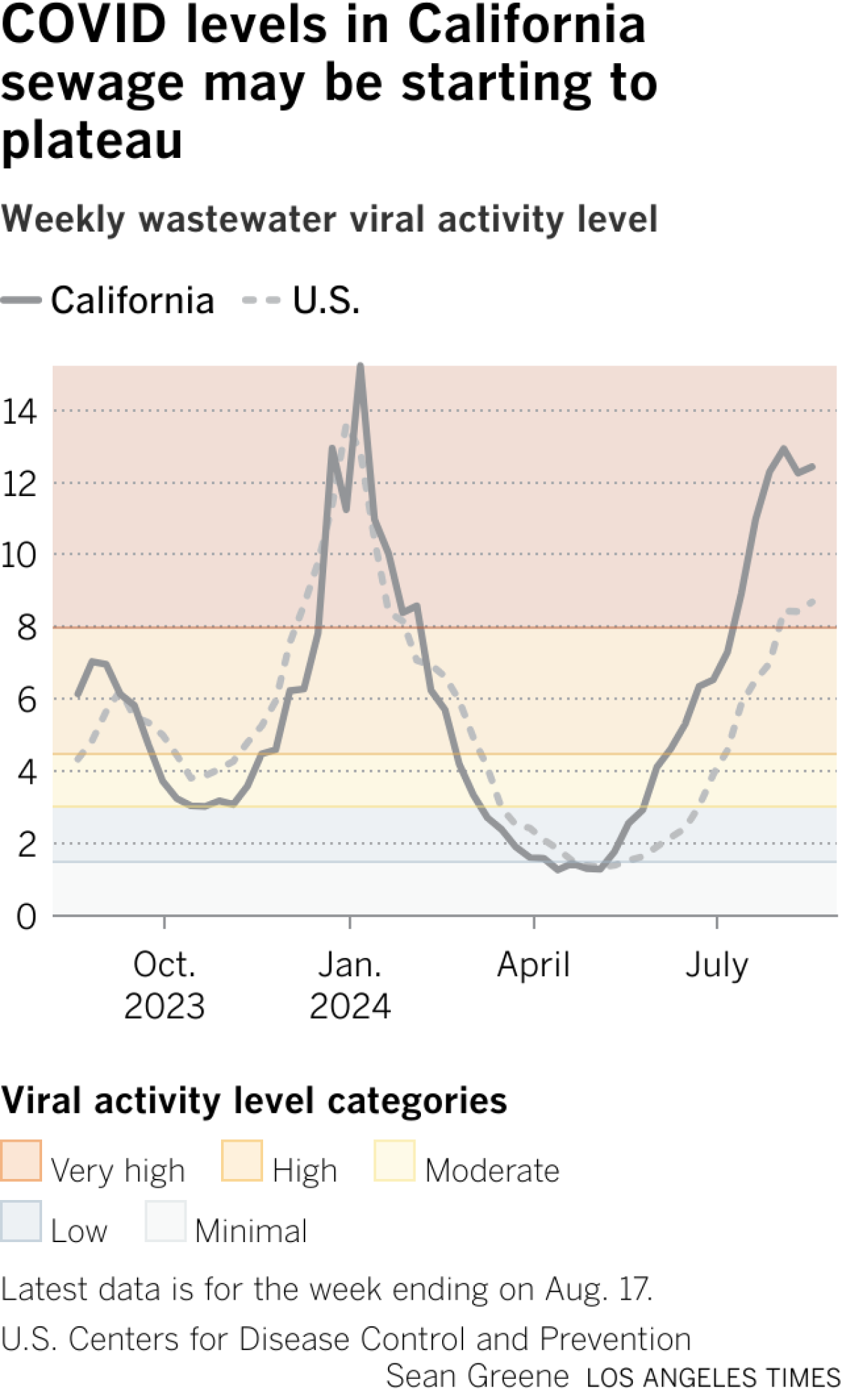
Doctors will be closely watching to see whether the back-to-school season and the Labor Day holiday weekend worsen the surge. Last week, officials with the U.S. Centers for Disease Control and Prevention said some data suggest a slowing of new coronavirus infections in some parts of the country. But a dip in the summer surge won’t be obvious until there are several weeks of sustained declines — which hasn’t happened yet.
Packed airports and large indoor events have long been shown to increase the spread of the coronavirus, and this summer has broken travel records. The Transportation Security Administration said June 23 resulted in the most passengers screened on a single day since the agency’s creation: 2.99 million. Southern California airports also have reported big increases in passenger volume.
Many DNC events occurred indoors, where the infection risk for large groups is greatest.
“That’s going to happen any time nearly 25,000 people are packed into an arena, in hotels and on shuttle buses for four days, no matter what the occasion is,” said California Democratic Party spokesperson Robin Swanson. “But the biggest takeaway from our convention is enthusiasm to elect Democrats across the country.”
Dr. Elizabeth Hudson, regional chief of infectious diseases at Kaiser Permanente Southern California, said her first thought as a physician in watching the DNC was, “Oh, no, hardly anyone is wearing a mask.”
She said she remembered thinking, “There’s probably going to be an awful lot of cases of COVID that come from this.
“You get a lot of people together in an indoor area who are talking and laughing and shouting, which is actually a more efficient way to spread COVID,” Hudson said. “Between all of that … exposure time, definitely, we are certainly going to see COVID.”
Even though masks have gone out of fashion, they remain an effective tool in helping to prevent COVID-19, along with avoiding sick people, spending more time outdoors or in well-ventilated areas, washing or sanitizing your hands frequently and staying up to date on vaccinations.
“When you are traveling, if you’re going to be in an indoor area with an awful lot of people, to really reduce your your risk of becoming COVID-positive, you really should be wearing a mask,” Hudson said.
And “if you’re on a plane, if you’re in an airport, those are the times you really want to make sure that you are wearing a mask,” she added.
The updated COVID-19 vaccinations for the 2024–25 season are expected to become available as soon as this week, and everywhere sometime in September.
There are a number of reasons why this summer’s COVID wave has been surprisingly strong.
One is the emergence of successive hyperinfectious coronavirus subvariants. In the spring, some of the subvariants collectively nicknamed FLiRT, including KP.2, began a midyear wave. That was followed by ever-more-contagious successor subvariants — KP.3 (nicknamed FLuQE, pronounced “fluke”) — and the latest, KP.3.1.1 (nicknamed deFLuQE).
With KP.3.1.1, “the particular variation that came up in this mutation was a little different than what people had seen with either natural immunity or with the vaccinations that we had available,” Hudson said.
“Because of that, it just made it much more easy to come into a population where people’s natural and vaccine-induced immunity was at a nadir,” Hudson said, with many people nearly a year or more out from their last immunization or their last COVID-19 illness.
There are now 26 states, including California, where COVID-19 is projected to be “growing” or “likely growing.” That’s down from 44 states about six weeks ago, according to the CDC.
The rate at which coronavirus tests are coming back positive continues to rise in California. For the week that ended Aug. 19, 14.4% of reported tests were positive. That’s higher than the peaks seen last summer and winter, and up from about 11.5% a month ago.
Overall, coronavirus levels in California’s wastewater have been largely flat in recent weeks, but remain at the season’s highest level.
How to protect yourself
- Test if you’re sick — and test daily. It’s sometimes taking longer after the onset of illness for a rapid test to show positive. If an initial test is negative, you may still have COVID. Consider retaking tests daily, up to five days after the onset of cough-and-cold symptoms, Hudson said. A positive test can help you take measures to isolate quicker and limit spread of the illness.
- Have a plan to ask for Paxlovid if you become ill. Paxlovid is an antiviral drug that, when taken by people at risk for severe COVID-19 who have mild to moderate symptoms, reduces the risk of hospitalization and death. There are also other anti-COVID drugs, such as molnupiravir, which is also taken orally, and remdesivir, which is administered intravenously.
- People who are moderately or severely immunocompromised can also get a medicine called pemivibart, whose brand name is Pemgarda. Given intravenously in a medical facility over an hour, the drug helps prevent COVID-19 before someone is exposed to the virus, but doesn’t replace vaccines.
- Wearing a mask, particularly on a crowded flight or other indoor venues, can help reduce the risk of infection.
- The CDC says people should stay away from others until at least 24 hours after their symptoms are getting better and they have not had a fever (and are not using fever-reducing medicine). The agency suggests taking added precautions for five days — like wearing a well-fitting mask and continuing to test for COVID, in case of viral rebound — to avoid sickening other people.
- Besides the CDC guidance, the Los Angeles County Department of Public Health also recommends testing yourself using a rapid test, and getting a negative result, before leaving isolation. The agency recommends masking for 10 days around other people after you start feeling sick, or if asymptomatic, your first positive COVID test. You can unmask earlier if you have two sequential negative COVID tests, taken at least a day apart. The agency also suggests staying away from the elderly and immunocompromised people for 10 days after you start to feel sick.
-
Generally, tips like these also reduce the risk of a coronavirus infection: keeping distance from other people, increasing air circulation by opening windows, turning on air purifiers, gathering outdoors if meeting with people, and sticking with enhanced hygiene: washing and sanitizing hands often, cleaning high-touch surfaces, and covering coughs and sneezes.
Additional travel tips from the CDC
- Make sure you are up to date on all of your routine vaccines; they protect from infectious diseases, such as measles, that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not common in the United States but are still common in other countries.
- Get up to date with your COVID-19 vaccines and get a seasonal flu vaccine. In the U.S., the CDC recommends getting COVID and flu vaccines in September or October.
- Prepare a travel health kit with items you may need, especially those that may be difficult to find at your destination. Include prescriptions and over-the-counter medicines and take enough to last your entire trip, plus extra in case of travel delays. Depending on your destination, you may also want to pack a mask, insect repellent, sunscreen (SPF 15 or higher), aloe, alcohol-based hand sanitizer, water disinfection tablets and your health insurance card.
Mehta reported from Chicago and Lin from San Francisco.